Key Learning Points
Corneal warpage is a reversible change in corneal shape—most often triggered by long‑term soft or rigid contact‑lens wear—and can mimic keratoconus on topography.
Typical warning signs include blurred or fluctuating vision, ghost images, halos, and poor lens comfort—especially after lens removal.
A “contact‑lens holiday,” careful follow‑up topography, and eventual refitting with healthier lenses or spectacles are the cornerstones of treatment.
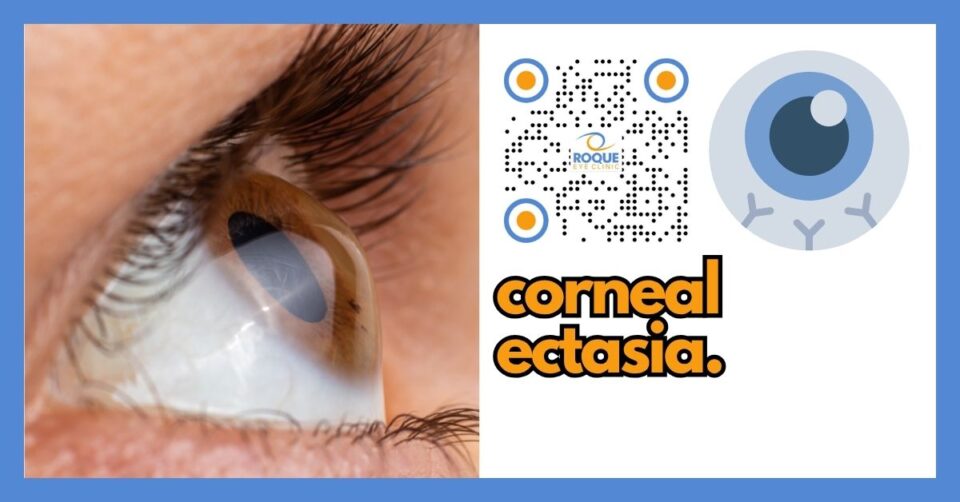
Differentiating warpage from true ectasia hinges on epithelial versus stromal changes: warpage shows focal epithelial thickening without stromal thinning.
Prevention revolves around high‑oxygen, well‑fitting lenses, strict hygiene, and scheduled “no‑lens” days.
Full visual recovery usually occurs within 2–12 weeks of stopping lens wear, but some corneas need up to five months.
Introduction – “When Your Windshield Warps”
Imagine your cornea as the clear front window of a camera. When we press a soft plastic mold against that window every day (a contact lens), gentle pressure and poor oxygen can warp the glass. The picture (your vision) blurs—not because the camera is broken but because the window has temporarily changed shape. This temporary distortion is called corneal warpage.
What Exactly Is Corneal Warpage?
Corneal warpage—sometimes labeled pseudokeratoconus—is a non‑inflammatory, usually reversible molding of the corneal surface caused by chronic mechanical or hypoxic stress, most frequently from ill‑fitting or low‑DK/t contact lenses. The warped zone often steepens and produces irregular astigmatism, higher‑order aberrations, and reduced contrast sensitivity.
Who Is at Risk?
| Risk Factor | Why it Matters |
|---|---|
| Low‑oxygen hydrogel or PMMA lenses | Less oxygen → tissue edema, shape change. |
| Long daily wear (>12 h) or overnight wear | Mechanical pressure and hypoxia accumulate. |
| High minus power or thick lenses | Greater weight and stiffness mold the cornea. |
| Cosmetic (circle) lenses | Pigmented layers raise roughness and toxicity. |
| Poor hygiene & solution toxicity | Inflammation exacerbates distortion. |
| Undiagnosed dry eye or allergy | Increases lens intolerance and corneal stress. |
Symptoms in Plain English
Vision that’s clear in the morning but smudgy by evening
Double or ghost images even with the lens out
Halos around lights at night
Sensation that lenses “never quite center”
Mild eye fatigue or headaches from squinting
How Your Doctor Confirms the Diagnosis
Detailed History – lens type, wear schedule, solutions.
Topography/Tomography – characteristic focal steepening with epithelial thickening but without stromal thinning distinguishes warpage from keratoconus.
Epithelial Thickness Mapping (OCT) – confirms thick epithelium.
Repeat Scans after Lens Holiday – progressive return to normal confirms warpage. Resolution timeline helps determine safe surgery dates.
Treatment—Letting the Cornea “Breathe and Bounce Back”
| Step | Everyday Analogy | Typical Duration |
|---|---|---|
| Stop lens wear | “Taking off tight shoes to let feet regain shape.” | 2–12 weeks (rarely up to 5 mo). |
| Refraction with glasses | Backup eyewear keeps vision functional. | Immediate |
| Serial topography every 1–2 weeks | Like measuring cake rise in the oven—watch the curve settle. | Until two identical scans |
| Refit with high‑DK/t silicone‑hydrogel or scleral lenses | Switching from stiff leather to breathable athletic shoes. | After corneal stability |
| Manage dryness/allergy | Lubricants, antihistamines, lid hygiene reduce stress. | Ongoing |
| Consider rigid gas‑permeable (RGP) or ortho‑k only if medically necessary | Use the right mold, not the wrong one. | Specialist discretion |
If you’ve been told your cornea is warped, remember it’s like a pillow that’s been flattened—give it time, rest, and fresh air, and it will fluff back up.
Prevention Tips You Can Start Today
Choose breathable lenses (silicone‑hydrogel, DK/t ≥ 100).
Follow the 20/20/20 rule for lenses: every 20 days, enjoy at least 20 consecutive “no‑lens” waking hours.
Strict hygiene: rub‑and‑rinse, fresh multipurpose or peroxide solutions, never top‑off.
Replace lenses and cases on schedule.
Never sleep, swim, or shower in contacts unless specifically approved.
Schedule annual lens‑fit checks and topography.
Treat dryness and allergies early.
What to Expect After Healing
Vision steadily clears as corneal maps normalize.
Surgery timing: Refractive or cataract surgery can be safely planned once two successive maps match (usually ≥2 weeks apart).
Return to lenses: Only after a professional re‑fit; ignoring this step risks a relapse.
Ten Frequently Asked Questions
| Question | Answer |
|---|---|
| 1. Is corneal warpage permanent? | No—over 90 % of cases fully reverse once lenses are stopped. |
| 2. Does warpage turn into keratoconus? | No, but the topography can look similar; true keratoconus shows stromal thinning. |
| 3. How long must I leave my lenses out? | Most corneas normalize in 2–12 weeks; your eye doctor will confirm with scans. |
| 4. Can I speed up recovery? | Rest, preservative‑free lubricants, and moist‑heat eyelid hygiene help comfort but cannot rush tissue remodeling. |
| 5. Will glasses correct my vision during healing? | Yes—temporary spectacles or daily disposable lenses with low wear time keep you functional. |
| 6. Are scleral lenses safer? | Properly fitted scleral lenses vault the cornea and deliver high oxygen, making warpage unlikely. |
| 7. May I wear cosmetic lenses again? | Only if they meet modern oxygen standards (DK/t), fit well, and you follow hygiene rigorously. |
| 8. Is LASIK still possible? | Yes—after stable maps. Warpage must fully resolve to avoid erroneous ablation. |
| 9. What if my cornea doesn’t return to normal? | Rarely, residual irregularity persists; rigid lenses or topography‑guided PRK may be considered. |
| 10. How do I know which cleaning solution is best? | High‑quality peroxide systems reduce preservatives that may contribute to toxicity. Ask your optometrist. |
Take‑Home Message
Corneal warpage is your cornea’s way of saying it needs a breather. With a lens holiday, medical guidance, and smarter lens choices, the cornea almost always snaps back to its natural shape—restoring crisp vision and opening the door to safe refractive surgery when desired.
Bibliography
1. Epidemiology & Risk
Wilson SE, et al. Soft contact lens–induced corneal warpage. CLAO J. 1998;24(3):140‑5.
Han SB, et al. Influence of soft contact lens material on corneal warpage. Eye Contact Lens. 2018;44(4):257‑63.
Holden BA, et al. Effects of long‑term extended contact lens wear on the human cornea. Invest Ophthalmol Vis Sci. 1985;26(11):1489‑501.
2. Diagnosis
Reinstein DZ, et al. Distinguishing contact lens warpage from ectasia: epithelial thickness mapping. J Cataract Refract Surg. 2017;43(6):827‑37.
Wu H, et al. Corneal warpage caused by cosmetic contact lenses: a case report. BMC Ophthalmol. 2023;23:17.
3. Natural History
Kim J, et al. Corneal stability after discontinued soft contact lens wear. Cont Lens Anterior Eye. 2008;31(4):182‑6.
Black IE, et al. Time course of reversal in contact lens–induced corneal distortion. Optom Vis Sci. 2002;79(10):636‑40.
4. Management
Dublin IT. Soft Contact Lens–Induced Corneal Warpage. Thesis, Technological Univ Dublin; 2019.
Littmann H, et al. Cessation of contact lenses prior to corneal tomography for refractive surgery screening. Eye (Lond). 2024;38:1558‑64.
5. Prevention & Patient Guidance
National Eye Institute. Contact Lenses: Healthy Vision Factsheet. NEI; 2024.
Review of Contact Lenses Editorial Board. May/June 2024 issue. Rev Cornea Contact Lenses. 2024.
BOOK AN APPOINTMENT
It takes less than 5 minutes to complete your online booking. Alternatively, you may call our BGC Clinic, or our Alabang Clinic for assistance.